Introduction:
Acute Myeloid Leukemia (AML) is a difficult to treat, life threatening malignancy with overall survival remaining extremely poor, approximately 15% at 5 years. Recent advances in therapeutic approaches for AML have significantly improved outcomes, most notably venetoclax and azacitidine which induces a remission in approximately 70% of patients. Despite this, the majority of patients ultimately relapse and succumb to their disease. We and others have previously shown that more monocytic (M5 by FAB classification) AML cells demonstrate increased resistance to venetoclax therapy and that relapse after venetoclax and azacitidine treatment shows a monocytic phenotype in approximately 30% of patients (Pei, et. al. Cancer Discovery, 2020). These patients experience decreased overall survival compared to patients with non-M5 AML. Furthermore, we have demonstrated that AML with a dominant monocytic phenotype can arise from a unique subclass of leukemia stem cells (LSCs) that we have termed monocytic-LSCs (m-LSCs) due to their immunophenotype, including expression of CD64. m-LSCs are highly resistant to venetoclax-based therapies (Pei, et. al., Cancer Discovery, 2023). As venetoclax is increasingly utilized in AML treatment regimens, it is essential to identify methods of targeting this m-LSC subtype to prevent and treat relapsed and refractory disease.
Methods:
To more effectively target monocytic AML, we have developed a novel chimeric antigen receptor (CAR) T cell therapy targeting CD64, an antigen commonly expressed in monocytic cells and strongly expressed in the m-LSC population. We generated two second-generation CAR constructs targeting CD64, one with CD28 and the other with 41BB costimulatory domains. We expressed these CARs in healthy donor human T cells via lentiviral transduction and tested their function in vitro and in vivo.
Results:
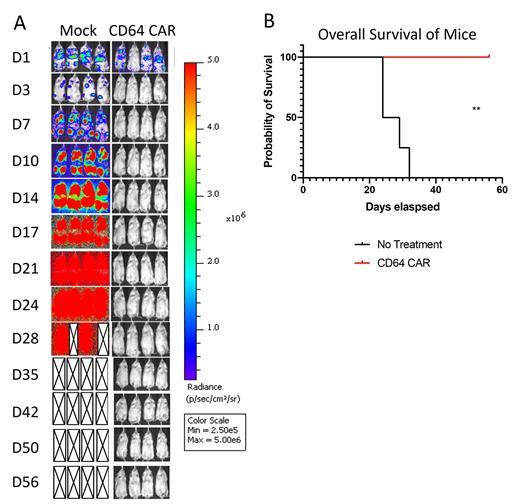
We demonstrate that CD64 CAR-T cells effectively treat monocytic AML using pre-clinical models. CD64 CAR-T cells eliminate CD64+ leukemia cell lines in vitro in a dose dependent manner with an effector to target (E:T) ratio of 1:4 and higher eliminating 100% of Molm14 leukemia cells at 18 hours compared to 0-10% in mock T-cell controls. We also show that CD64 CAR-T cells eliminate established Molm14 leukemia in vivo, with 100% of CAR-T treated mice surviving over 50 days with no evidence of leukemia versus less than 30 days survival with high tumor burden in mock treated mice (p<0.01, Figure 1). We find that CD64 CAR-T cells with CD28 verses 41BB costimulatory domains are similarly efficacious against monocytic AML, though we find more prolonged persistence of CD64-41BBz CAR-T cells in mice with long term leukemia free survival. Furthermore, we demonstrate that CD64 CAR-T cells kill CD64+ primary patient derived AML cells in ex vivo co-culture, resulting in a 60-80% reduction in viable AML cells at 18 hours across 1:1 to 1:16 E:T ratios compared to mock T cell controls. We further show that CD64 CAR-T cells target m-LSCs and reduce the engraftment potential of primary AML cells in mice with a nearly 9-fold reduction in leukemia burden in CAR-T treated versus control mice. Finally, preliminary experiments with AML patient derived xenograft models further support the in vivo efficacy of CD64 CAR-T cell treatment.
Conclusions:
Our data provide promising preclinical evidence for the efficacy of a novel CD64 CAR-T therapy in the treatment of monocytic AML. We propose that using this regimen to augment AML therapy is a potentially powerful means to eradicate m-LSCs, which are inherently resistant to venetoclax, and thereby increase remission duration. This concept serves as the basis for an upcoming clinical trial of CD64-directed CAR-T cells for CD64 expressing AML.
Figure 1: CD64 CAR-T cells eliminate AML in in vivo murine leukemia models. A) NSG mice leukemia models of GFP expressing Molm14, a CD64+ human leukemia cell line, experience leukemia clearance within 3 days after treatment with CD64-28z CAR-T cells, as shown by decreased bioluminescent signal in images of CAR-T treated mice. Mock transduced human T-cells from the same human donor serve as a control. B) Survival curves demonstrate 100% survival of CAR-T treated mice over the experiment (p<0.01).
Disclosures
Jordan:AML JV: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal